Customized Distal Tibial Cage
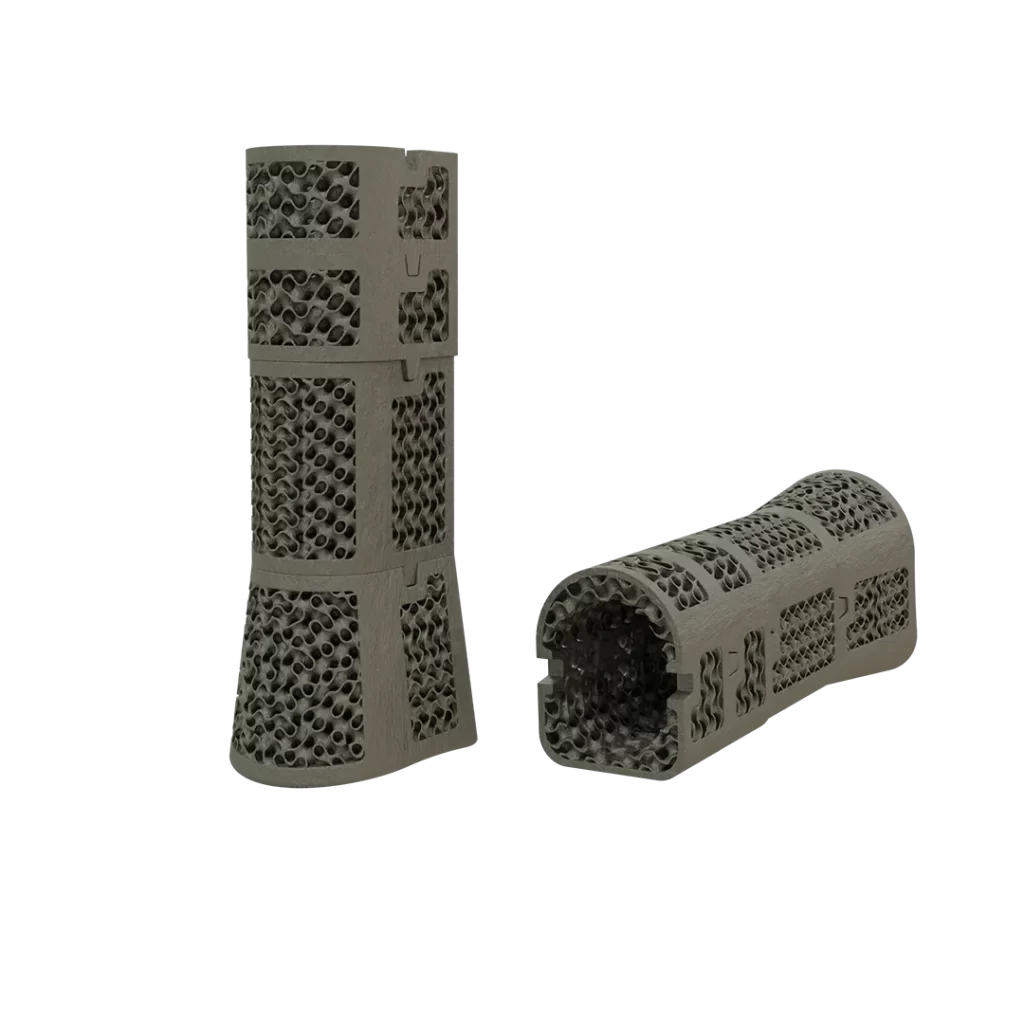
For cases with large bone defects from trauma or tumors, the customized distal tibia cages are designed to fit the intramedullary nail used by the physician and to replace the bone defect. They feature a porous structure for better osseointegration.
Product Overview


Product Overview
Before the advent of 3D printing technology, vascularized fibular transfer, allograft and autograft spacers, and the cumbersome method of moving bone pieces with external fixation and braces were used in cases of severe bone defects.
As the tibiotalar joint was damaged, an intramedullary hole was designed in the customized distal tibia cage to allow for the passage of the tibia-talo-calcaneal (TTC) nail to maintain postoperative compression across the joint surfaces.
However, customized distal tibial cages are designed based on the surgeon’s preoperative planning while taking into account the unique geometry of the patient’s bone and any defects that may be present. This leads to a great surgical outcome and reduced stress for the surgeon as everything has been determined preoperatively and conforming prostheses have been manufactured accordingly.
Workflow
Imaging
CT scan and X-ray imaging are acquired to create an accurate 3D model of the patient's lower extremity, and identify the extent of the defect.
Implant Design
Clinical engineers design a custom implant based on the patient's anatomy and the intramedullary nail being used.
Product Manufacturing
Upon physician approval, the implant is manufactured using 3D printing technology.
Surgery
The sterilized implant is delivered to the attending physician along with an anatomical model of the patient. A company representative may be present in the operating room to assist with cage placement.
Specifications
Surgeons can collaborate with the engineering team to design the implant’s geometry and features based on their clinical assessment of the patient and the intended treatment plan.
At the interface between the bone and the prosthesis, it is possible to have a TPMS lattice structure such as a gyroid, to promote bone ingrowth as a secondary mechanism of fixation.
The prosthesis is designed based on the axial geometry of the bone shaft to fit perfectly on the bone and promote osseointegration.
The height of the cages is made according to the opposite limb to prevent limb shortening.
Specifications
Surgeons can collaborate with the engineering team to design the implant’s geometry and features based on their clinical assessment of the patient and the intended treatment plan.
benefits
Lorem ipsum dolor sit amet, it amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.Lorem , luctus nec ullamcorper mattis, pulvinar dapibus leo.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
- Lorem kjsae ismcp ipsum
- Lorem ipsur sit amet
- fast and hard
- easy and flex

Cases report
The patient is a 31-year-old man diagnosed with pelvic osteosarcoma, who presented with...Read More
The patient is a 36-year-old man who has been diagnosed with pelvic sarcoma...Read More
The patient is a 22-year-old woman who has been affected by a Giant...Read More
The patient is a 49-year-old man who had previously undergone surgery and subsequently...Read More
Cases report
Our case reports highlight successful outcomes achieved through our custom-made implants. They showcase the effectiveness of our treatment plans and the expertise of our team in creating tailored solutions for each patient.
By reviewing these reports, you can gain a better understanding of the level of care and precision that we bring to every aspect of our work with patient specific implants.




